
The real talk about DIABETES.
Diabetes happens when the body doesn’t make enough insulin, doesn’t make any insulin at all, or when your body doesn’t respond to insulin the way it’s supposed to. Insulin has an important job in lowering your blood sugar level, so when you have type 2 diabetes, your body has a tougher time managing your blood sugar.
First, let me tell you what happens with sugar:
- When you eat, some of your food is broken down into sugar
- Sugar enters your blood
- Then it travels through your blood to all of your cells. Sugar isn’t always a bad thing! Your body needs that sugar for energy
Next, here’s what’s going on with insulin:
- Insulin is a hormone made by the beta cells in your pancreas
- Insulin is like a key that helps unlock cells and lets the sugar into the cells to give them energy
- When sugar moves out of your blood and into your cells, the amount of sugar in your blood goes down
Managing diabetes so it works for you
Listen, people managing diabetes should want to control their blood sugar, and that means living a healthy, active life. I know I do! It’s important that you work with your docs and other health care providers to build a personalized diabetes care plan that includes healthy eating, physical activity, tracking your blood sugar, and taking your medicine as prescribed by your health care provider.
If you feel frustrated coping with diabetes, you’re not alone. I went through this myself, and I reached out to friends and family to help. My advice is to get connected to your community. Recognize that these feelings are normal, and learn healthy ways to manage them.
Insulin Therapy
Because the hallmark of type 1 diabetes is absent or near-absent β-cell function, insulin treatment is essential for individuals with type 1 diabetes. In addition to hyperglycemia, insulinopenia can contribute to other metabolic disturbances like hypertriglyceridemia and ketoacidosis as well as tissue catabolism that can be life threatening. Severe metabolic decompensation can be, and was, mostly prevented with once or twice daily injections for the six or seven decades after the discovery of insulin. However, over the past three decades, evidence has accumulated supporting more intensive insulin replacement, using multiple daily injections of insulin or continuous subcutaneous administration through an insulin pump, as providing the best combination of effectiveness and safety for people with type 1 diabetes. The Diabetes Control and Complications Trial (DCCT) demonstrated that intensive therapy with multiple daily injections or continuous subcutaneous insulin infusion (CSII) reduced A1C and was associated with improved long-term outcomes (1–3). The study was carried out with short-acting (regular) and intermediate-acting (NPH) human insulins. In this landmark trial, lower A1C with intensive control (7%) led to ∼50% reductions in microvascular complications over 6 years of treatment. However, intensive therapy was associated with a higher rate of severe hypoglycemia than conventional treatment (62 compared with 19 episodes per 100 patient-years of therapy). Follow-up of subjects from the DCCT more than 10 years after the active treatment component of the study demonstrated less macrovascular as well as less microvascular complications in the group that received intensive treatment (2,4).
Over the last 25 years, rapid-acting and long-acting insulin analogs have been developed that have distinct pharmacokinetics compared with recombinant human insulins: basal insulin analogs have longer duration of action with flatter, more constant plasma concentrations and activity profiles than NPH insulin; rapid-acting analogs (RAA) have a quicker onset and peak and shorter duration of action than regular human insulin. In people with type 1 diabetes, treatment with analog insulins is associated with less hypoglycemia and weight gain as well as lower A1C compared with human insulins (5–7). More recently, two new injectable insulin formulations with enhanced rapid action profiles have been introduced. Inhaled human insulin has a rapid peak and shortened duration of action compared with RAA and may cause less hypoglycemia and weight gain (8), and faster-acting insulin aspart and insulin lispro-aabc may reduce prandial excursions better than RAA (9,9a,9b); further investigation is needed to establish a clear place for these agents in diabetes management. In addition, new longer-acting basal analogs (U-300 glargine or degludec) may confer a lower hypoglycemia risk compared with U-100 glargine in patients with type 1 diabetes (10,11). Despite the advantages of insulin analogs in patients with type 1 diabetes, for some patients the expense and/or intensity of treatment required for their use is prohibitive. There are multiple approaches to insulin treatment, and the central precept in the management of type 1 diabetes is that some form of insulin be given in a planned regimen tailored to the individual patient to keep them safe and out of diabetic ketoacidosis and to avoid significant hypoglycemia, with every effort made to reach the patient’s glycemic targets.
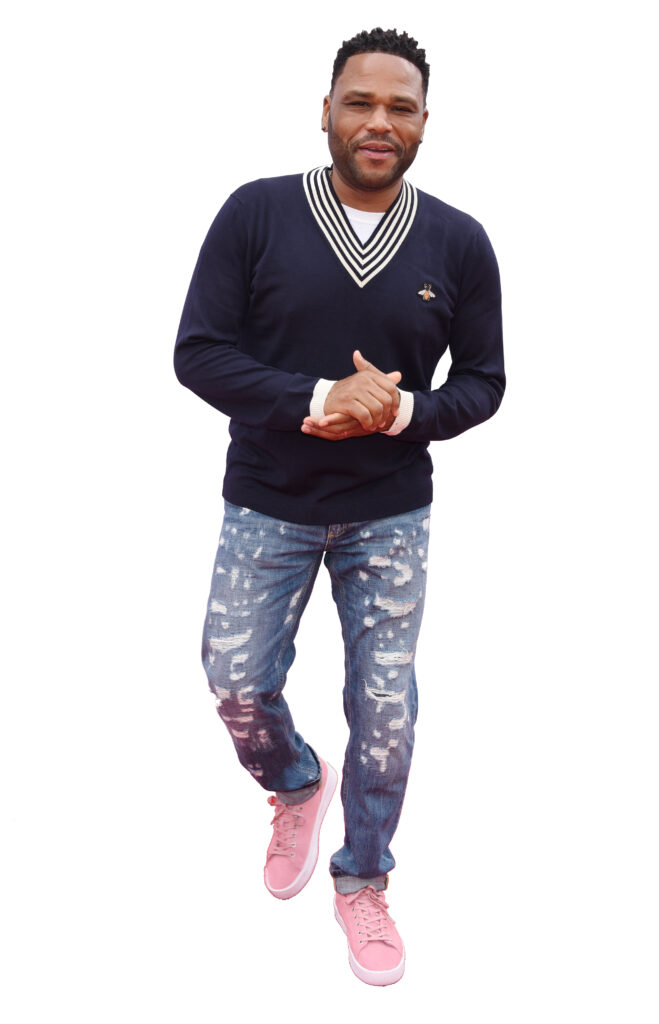
Star of ABC’s black-ish
Diagnosed with type 2 diabetes in 2002



 Sofia Llamas: A Force for Good in Colorado – Igniting Hope and Empowering Communities
Sofia Llamas: A Force for Good in Colorado – Igniting Hope and Empowering Communities  Yella Beezy Released on $750,000 Bond
Yella Beezy Released on $750,000 Bond 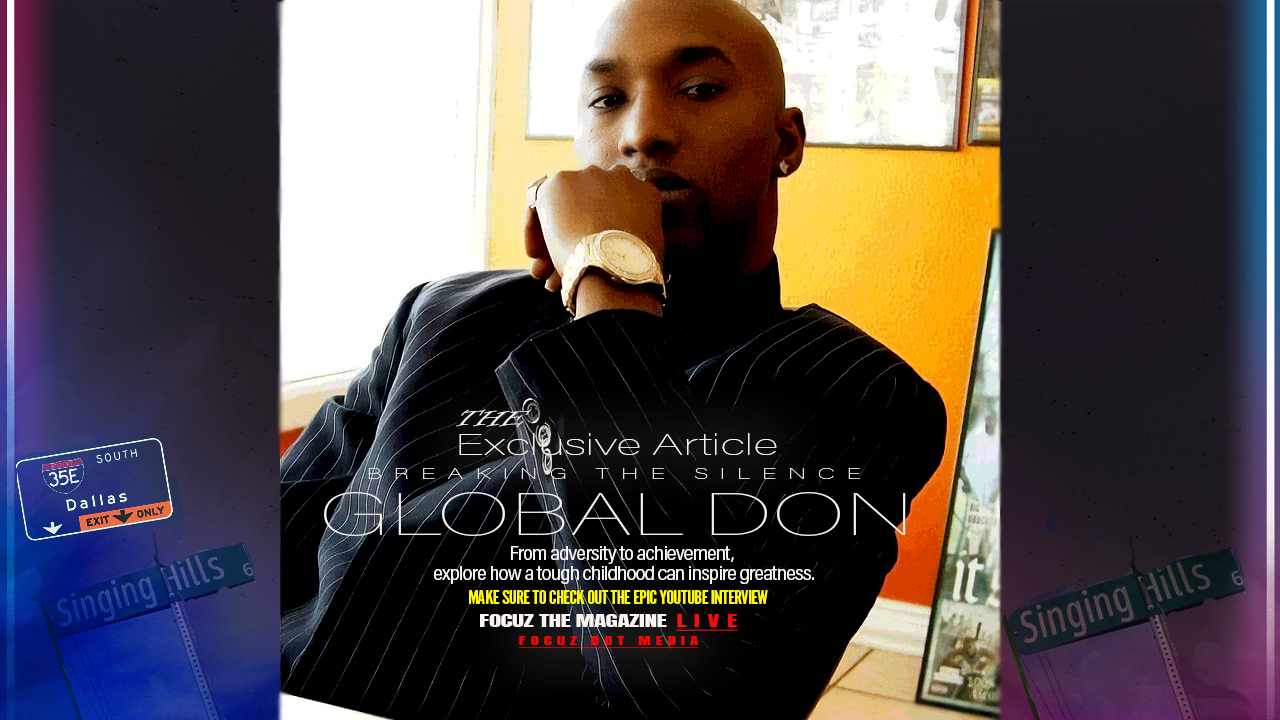 Global Don Breaking The Silence
Global Don Breaking The Silence  Was it really about the Lil Wayne Concert
Was it really about the Lil Wayne Concert  South Florida residents told to steer clear of ‘life-threatening’ flooding
South Florida residents told to steer clear of ‘life-threatening’ flooding  Camping 4 Beginners
Camping 4 Beginners  Trump administration offers to pay plane tickets, give stipend to self-deporting immigrants
Trump administration offers to pay plane tickets, give stipend to self-deporting immigrants 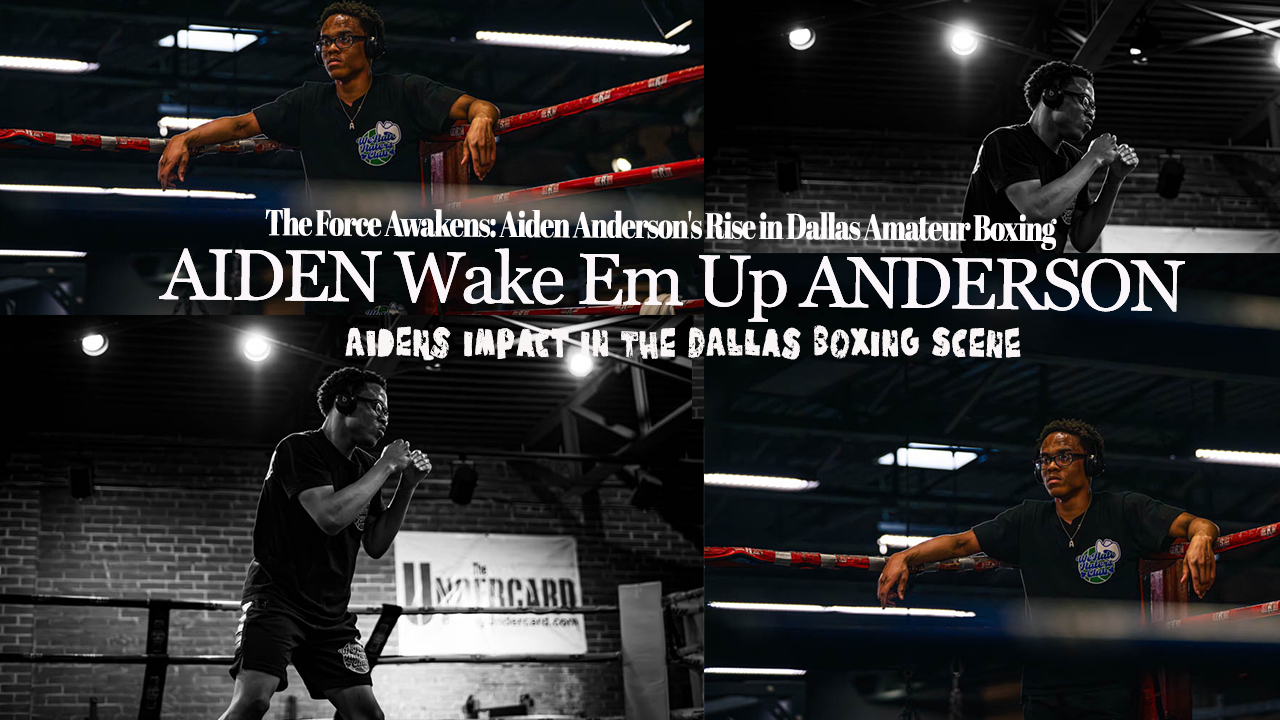 The Force Awakens: Aiden Anderson’s Rise in Dallas Amateur Boxing
The Force Awakens: Aiden Anderson’s Rise in Dallas Amateur Boxing 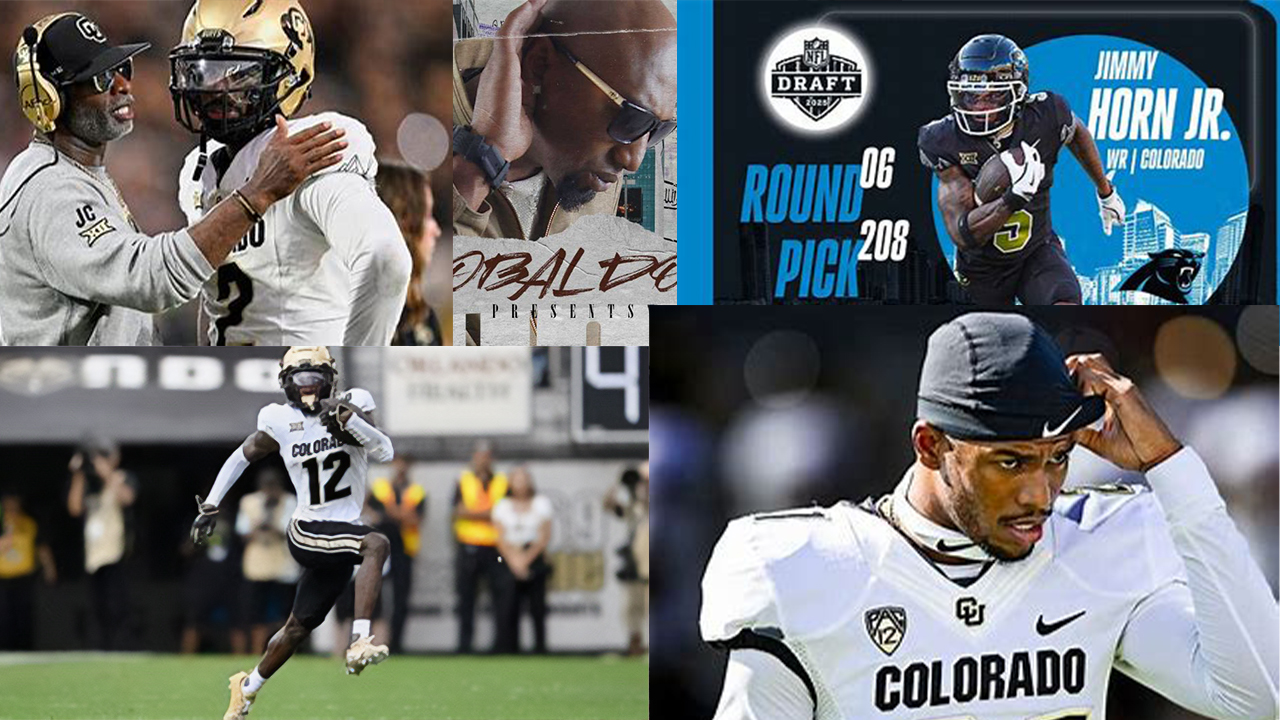 Thomas Edward Patrick Brady Jr, Shedeur Sanders, Travis Hunter, Shilo Sanders, Jimmy Horn Jr, Global Don, and more
Thomas Edward Patrick Brady Jr, Shedeur Sanders, Travis Hunter, Shilo Sanders, Jimmy Horn Jr, Global Don, and more